We believe that integrated nonprofit medical systems that share a commitment to providing access to high-quality care for our communities, as well as training the healthcare workforce of the future, should have the support they need to remain sustainable.
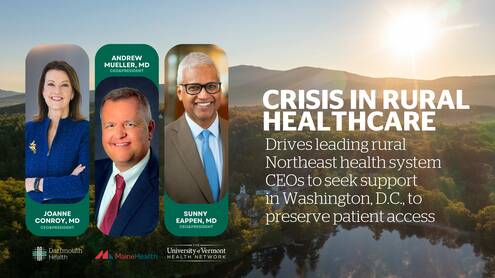
Joanne M. Conroy, MDRural Americans are more likely to develop chronic illnesses and die compared to their urban counterparts. Across the country, accessing care to maintain health is harder than ever. At the end of July, the three CEOs of leading rural academic health systems in the northeast told federal lawmakers that new policies, programs and payments are needed to ensure patients in rural communities are able to get the high-quality care they need, when and where they need it.
Dartmouth Health, MaineHealth and University of Vermont Health Network share similar academic missions, healthcare service delivery models, support for research and innovation, nonprofit statuses, and deep commitments to the communities they serve. The patients in their rural communities face common challenges – growing older, suffering from chronic disease, unmet behavioral and mental health needs, and a lack of affordable housing, among others. Ongoing workforce shortages and reimbursements from Medicare and Medicaid that do not cover the cost of providing care compound the challenges of preserving access to vital services.
Working with Congress to support patients in rural America
“We are bringing the critical needs of our patients and our communities to Washington, D.C., and proposing solutions to ensure that the people of northern New England and northern New York can get the high-quality care they deserve in our region, now and into the future,” said Sunny Eappen, MD, MBA, president and chief executive officer of UVM Health Network. “We appreciate our Congressional delegations’ willingness to hear about the big challenges uniquely impacting rural communities here and across the nation.”
The federal government can take steps to preserve access to care in rural areas. Northern New England and northern New York health system leaders discussed solutions with their Congressional delegations, including proposals that would increase access, increase funding from Medicare, and reduce regulatory burdens, allowing more flexibility in providing care. The proposed changes would be measured for success.
“We know what we must do to take care of our patients and communities,” said Joanne M. Conroy, MD, chief executive officer and president of Dartmouth Health. “We believe that integrated nonprofit medical systems that share a commitment to providing access to high-quality care for our communities, as well as training the healthcare workforce of the future, should have the support they need to remain sustainable. Equitable access to quality healthcare in our rural regions depends upon it.”
“As a family physician by training, it has been difficult to watch our rural communities struggle to maintain access to high-quality care for their residents,” said Andrew Mueller, MD, chief executive officer of MaineHealth. “Our proposals align with, and support, our MaineHealth vision of ‘Working together so our communities are the healthiest in America.’”
Current challenge: Improving access is at odds with managing cost for rural health systems
As the primary providers of healthcare in the region, the three systems step in to provide critical patient services that lose money, such as primary care, behavioral and mental health, ambulance services, long-term care and dialysis. Without change, it will become increasingly difficult for nonprofit safety net hospitals to meet the needs of patients.
All three systems believe that cost should not prevent anyone from getting the care they need, and have strong financial assistance policies to support patients. At the same time, they are working to improve access while working to manage expenses in the face of skyrocketing pharmaceutical costs, and the escalating cost of recruiting and retaining talented staff during a national workforce shortage.
However, under the current system, vital efforts to preserve and improve access to care are at odds with the urgent need to hold down the cost of that care. In Vermont, more patients are accessing health care services, which highlights progress being made on access. However, Vermont’s largest commercial insurer, Blue Cross Blue Shield of Vermont, blamed increased demand as a reason for their near-record-high premium increases, averaging 24% in 2025.
Enduring commitment: Providing vital support for patients and communities
In addition to participating in initiatives that aid in improving patient outcomes and reducing the total cost of care to patients, Dartmouth Health founded the Center for Connected Care (telehealth) in 2012 with a primary objective of helping deliver outstanding healthcare to the region independent of patient location. TeleHealth services were designed to drive accessible, efficient and effective care by complimenting and enhancing programs and services provided in local and regional communities. Connecting clinical expertise to distant sites via telemedicine improves quality of care and patient outcomes, lowers costs for patients and systems, and improves patient and provider satisfaction.
Vermont is the lowest-cost provider of care for Medicare in the nation, and UVM Medical Center is in the lowest-cost 25% of academic medical centers nationwide. In 2023, UVM Health Network supported more than 8,000 patients by covering the cost of $22 million in care, and helped more than 6,000 patients access free prescription medication, equipment and support, covering $7.5 million that would have come out of the pockets of low- and middle-income patients.
In spite of investing over $500 million last year to subsidize critical healthcare services that are under-reimbursed by payors, MaineHealth exceeded its $100 million budget savings target through purchasing contracts, improved care delivery models and administrative efficiencies. These efforts support MaineHealth’s commitment to maintaining an operating budget target of 3% or less, which supports the system’s mission of ensuring high-quality affordable care for its patients.
All three systems are deeply interconnected with and invested in their communities. All three systems are the largest private employers in their respective states, and are firmly committed to the people of the region. Dartmouth Health is formally designated as an anchor institution, highlighting investments in local and regional population health initiatives designed to keep communities thriving.
“This is a critical time to make changes that will support us in providing the high-quality care that our patients – their constituents – need and deserve,” Dr. Eappen said. “There is a lot of work to do from here, but we are looking forward to advancing these solutions at the federal and state level to ensure access for the people of our rural region, now and into the future.”
###
Contact:
MaineHealth: John Porter: john.porter@mainehealth.org
UVM Health Network: Annie Mackin: annie.mackin@uvmhealth.org
About Dartmouth Health
Dartmouth Health, New Hampshire’s only academic health system and the state’s largest private employer, serves patients across northern New England. Dartmouth Health provides access to more than 2,000 providers in almost every area of medicine, delivering care at its flagship hospital, Dartmouth Hitchcock Medical Center (DHMC) in Lebanon, NH, as well as across its wide network of hospitals, clinics and care facilities. DHMC is consistently named the #1 hospital in New Hampshire by U.S. News & World Report, and is recognized for high performance in numerous clinical specialties and procedures. Dartmouth Health includes Dartmouth Cancer Center, one of only 57 National Cancer Institute-designated Comprehensive Cancer Centers in the nation, and the only such center in northern New England; Dartmouth Health Children’s, which includes the state’s only children’s hospital and multiple locations around the region; member hospitals in Lebanon, Keene, Claremont and New London, NH, and Windsor and Bennington, VT; Visiting Nurse and Hospice for Vermont and New Hampshire; and more than 24 clinics that provide ambulatory and specialty services across New Hampshire and Vermont. Through its historical partnership with Dartmouth and the Geisel School of Medicine, Dartmouth Health trains nearly 400 medical residents and fellows annually, and performs cutting-edge research and clinical trials recognized across the globe with Geisel and the White River Junction VA Medical Center in White River Junction, VT. Dartmouth Health and its more than 13,000 employees are deeply committed to serving the healthcare needs of everyone in our communities, and to providing each of our patients with exceptional, personal care.