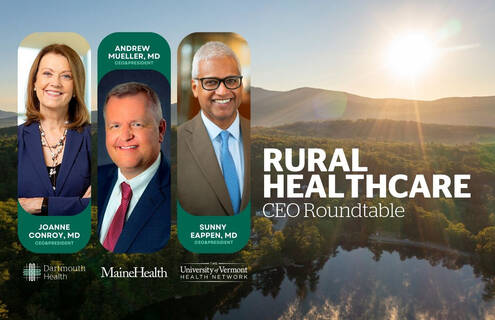
Dartmouth Health CEO and President Joanne M. Conroy, MD, joined MaineHealth CEO Andrew Mueller, MD, and The University of Vermont Health Network (UVMHN) President and CEO Sunny Eappen, MD, MBA in a roundtable discussion about the extreme crisis in rural healthcare on Monday, May 22, 2023.
The roundtable was live-streamed on YouTube from Dartmouth Health's Dartmouth Hitchcock Medical Center. The recording can be viewed on the Dartmouth Health YouTube channel. This content is cleared for use by media outlets on all broadcast and digital platforms.
"Seventy percent of hospitals nationwide were in the red in 2022, so we're not alone. In rural America, the challenges are more difficult to navigate, especially in New England where our systems are located, and which has not bounced back like other areas of the country post-COVID," said Conroy. "Although the [federal] provider relief funds were crucial and allowed our hospitals and rural hospitals to recover, post-recovery we are facing a host of challenges all at once, led by a persistent healthcare workforce shortage, which affects each of our institutions."
Conroy said labor costs continue to escalate primarily because organizations must pay premiums either for their own employees to work overtime to cover gaps, or they must pay contract labor – commonly referred to as ‘travelers' – often more than three times the rate that their own employees are paid. A reality that can contribute to employee discontent and attrition.
The leaders of the largest healthcare systems in northern New England and the North Country of New York discussed what it means to be an academic health system, the workforce challenges, including recruitment, housing and childcare, as well as payer, regulatory and inflation challenges, and innovations that preserve and improve access to high-quality care.
"Discussing our common challenges as rural health systems is so important, and by working together I am certain that we can preserve and improve access to high-quality care for patients in our region," said Sunny Eappen, MD, MBA, President and CEO of the UVM Health Network. "I do see a bright light in the face of this turmoil: We have an opportunity now to make truly positive lasting change while we chart a path forward. That means getting creative with the way we deploy our talented workforces, allowing our physicians, nurses, and all of our staff to work at their highest level; advancing telehealth in new, efficient and exciting ways that make scheduling appointments and getting answers easier for patients and providers; and leading the way as diverse, equitable and vibrant organizations. Of course to do all this, we will need the support of our federal and state governments, and we will need commercial payers to reimburse us at levels that allow us to continue providing care to their members, who are our patients."
As academic medical centers, Dartmouth Hitchcock Medical Center, Maine Medical Center and University of Vermont Medical Center are crucial 'safety nets' for New Hampshire, Maine and Vermont. While smaller critical access hospitals may close beds due to staffing challenges, the academic medical centers must keep beds open for the sickest and neediest patients that cannot be cared for in smaller facilities. The leaders agreed that labor costs have increased 12-15 percent post-pandemic, and these are costs that they are unable to pass along to consumers or insurance companies, which has created significant financial gaps for their systems.
"We're our state's largest private employers. And we have a big economic impact in terms of the ability to create jobs, to give people good pay, and to really help stimulate the economies of the states we serve," said Andrew Mueller, MD, Chief Executive Officer, MaineHealth. "If we are impacted to the point that we have to reduce services, not only do we run the risk of individuals being harmed by failure to access care, we also run the risk of really damaging some of our rural communities economically and socially."
Bipartisan Policy Center (BPC) President Bill Hoagland moderated the discussion and shared, "Although I work in Washington, DC, my heart and my family farm are back in Indiana, so I have a good sense as to the challenges that face rural America. Rural healthcare delivery is a critically important conversation to have here in New England and across the country, right now, before it's too late."
The purpose of the roundtable was to highlight the critical concerns, build awareness of the problems rural healthcare providers face across the country, discuss possible solutions, and draw attention to the fact that health systems like Dartmouth Health, UVMHN and MaineHealth cannot fix these problems alone.
About Dartmouth Health
Dartmouth Health, New Hampshire's only academic health system and the state's largest private employer, serves patients across northern New England. Dartmouth Health provides access to more than 2,000 providers in almost every area of medicine, delivering care at its flagship hospital, Dartmouth Hitchcock Medical Center (DHMC) in Lebanon, NH, as well as across its wide network of hospitals, clinics and care facilities. DHMC is consistently named the #1 hospital in New Hampshire by U.S. News & World Report, and recognized for high performance in numerous clinical specialties and procedures. Dartmouth Health includes its Dartmouth Cancer Center, one of only 51 National Cancer Institute-designated Comprehensive Cancer Centers in the nation, and the only such center in northern New England; Dartmouth Health Children’s, including the Children’s Hospital at Dartmouth Hitchcock Medical Center, the state’s only children’s hospital and clinic locations around the region; member hospitals in Lebanon, Keene and New London, NH, and Windsor, VT, and Visiting Nurse and Hospice for Vermont and New Hampshire; and more than 24 clinics that provide ambulatory services across New Hampshire and Vermont. Through its historical partnership with Dartmouth and the Geisel School of Medicine, Dartmouth Health trains nearly 400 medical residents and fellows annually, and performs cutting-edge research and clinical trials recognized across the globe with Geisel and the White River Junction VA Medical Center in White River Junction, VT. Dartmouth Health and its more than 13,000 employees are deeply committed to serving the healthcare needs of everyone in our communities, and to providing each of our patients with exceptional, personal care.
About MaineHealth
MaineHealth is a not-for-profit integrated health system whose vision is, "Working together so our communities are the healthiest in America." It consists of nine local hospital systems, a comprehensive behavioral healthcare network, diagnostic services, home health agencies, and more than 1,500 employed and independent physicians working together through the MaineHealth Medical Group. With approximately 22,000 employees, MaineHealth provides preventive care, diagnosis and treatment to 1.1 million residents in Maine and New Hampshire. It includes Franklin Memorial Hospital/Franklin Community Health Network in Farmington, LincolnHealth in Damariscotta and Boothbay Harbor, Maine Behavioral Healthcare in South Portland, MaineHealth Care at Home in Saco, Maine Medical Center in Portland, Memorial Hospital in North Conway, N.H., Mid Coast-Parkview Health in Brunswick, NorDx in Scarborough, Pen Bay Medical Center and Waldo County General Hospital in Rockport and Belfast, Southern Maine Health Care in Biddeford and Sanford, Spring Harbor Hospital in Westbrook and Stephens Memorial Hospital/Western Maine Health Care in Norway. MaineHealth Affiliates include Maine General Health in Augusta and Waterville, New England Rehabilitation Hospital in Portland and St. Mary's Regional Medical Center in Lewiston. It is also a significant stakeholder in the MaineHealth Accountable Care Organization in Portland.
About The University of Vermont Health Network
The University of Vermont Health Network is an integrated system serving the residents of Vermont and northern New York with a shared mission: working together, we improve people's lives. The partners are:
- The University of Vermont Medical Center
- The University of Vermont Health Network Medical Group
- The University of Vermont Health Network – Alice Hyde Medical Center
- The University of Vermont Health Network – Central Vermont Medical Center
- The University of Vermont Health Network – Champlain Valley Physicians Hospital
- The University of Vermont Health Network – Elizabethtown Community Hospital
- The University of Vermont Health Network – Porter Medical Center
- The University of Vermont Health Network – Home Health & Hospice
Our 15,000 employees are driven to provide high-quality, cost-efficient care as close to home as possible. Strengthened by our academic connection to the University of Vermont, each of our affiliates remains committed to its local community by providing compassionate, personal care shaped by the latest medical advances and delivered by highly skilled experts.