This page contains the following sections:
When is surgical repair or replacement of an aortic valve advisable?
How is repair or replacement of an aortic valve accomplished?
What are the risks and benefits of such surgery?
What is involved in a typical recovery?
When is surgical repair or replacement of an aortic valve advisable?
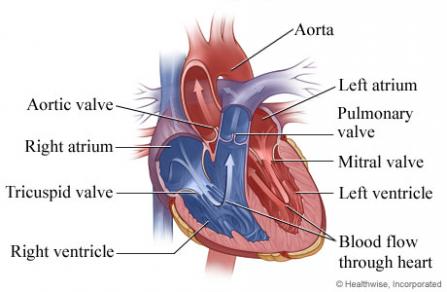
Your aortic valve is several little flaps of tissue that control the flow of blood from your heart's left ventricle into your aorta, the body's largest artery. If it's seriously diseased or defective, it may be advisable to consider the possibility of surgical repair.
If you are diagnosed with a damaged aortic valve, your surgeon will evaluate the specifics of your situation and help you weigh the risks of cardiac surgery against the risks of continuing to manage the disorder with medication and other nonsurgical treatments. In some circumstances, especially if your symptoms are not severe, they can be managed with lifestyle changes and/or medication. However, a disorder of the aortic valve that is severe or causes symptoms can only be fixed surgically; nonsurgical options will at best just delay the need for surgery.
Should you and your surgeon decide the time is right for surgery, keep in mind that our cardiac surgeons have considerable expertise in all the proven options for the surgical repair or replacement of damaged aortic valves. Surgery on the aortic valve is quite common.
How is repair or replacement of an aortic valve accomplished?
There are a number of ways to repair or replace a damaged or defective aortic valve. The two primary matters your surgeon will consider are whether your valve can be repaired or must be replaced, and which surgical approach will work best.
In certain limited circumstances, especially if your valve is leaky rather than blocked, it may be possible to repair it using small tissue patches on the flaps of the valve.
In most cases of surgery on a damaged aortic valve, however, replacement rather than repair will be the most advisable option. There are two primary kinds of replacement valves. Factors such as your age and the overall state of your health will affect which kind is most appropriate:
- Mechanical valves are made of very durable artificial materials, including titanium, carbon, polyester, Dacron and Teflon. They are typically very long-lasting; however, use of a mechanical valve usually requires patients to take blood-thinning medication (often referred to by the brand name of Coumadin) for the rest of their lives.
- Biological valves, also known as tissue valves or bioprosthetic valves, are made of animal tissue, often from a pig or a cow. They do not usually necessitate the lifelong use of blood-thinning medication; however, biological valves have a limited life span, averaging 10 to 20 years, so a second valve replacement operation may be required in the future. Biological valves are used in the majority of aortic valve replacement operations.
The appropriate surgical approach will depend on such factors as whether your valve can be repaired or must be replaced, how damaged it is, and the overall state of your health. Your surgeon will determine which of the following procedures is most appropriate in your particular situation:
- Open-heart surgery to repair or replace an aortic valve involves making a 7- to 10-inch incision over the middle of the sternum, or breastbone, then dividing the sternum to allow access to the heart. In some cases a less invasive option, involving a slightly smaller sternal incision, is possible. Then the damaged valve is either repaired or replaced.
It will be necessary to stop your heart from beating during the procedure, so the operation can be performed on a motionless and bloodless field; while your heart is stopped, a device known as a heart-lung bypass machine will take over your heart's function and maintain your circulation. Very occasionally, during complex operations involving the aorta, you may also be put into a state known as hypothermic circulatory arrest; this involves lowering your body temperature to significantly slow your body's cellular activity, permitting your blood flow to be temporarily stopped. (The term "hypothermic" comes from Greek words meaning "low heat," while "circulatory arrest" means your circulation is arrested, or stopped.) In other cases, a technique known as axillary cannulation (or the insertion of a drainage tube, known as a cannula, in an artery in your armpit, or axilla) can allow aortic surgery to be performed without hypothermic circulatory arrest; this advance may reduce the incidence of postoperative strokes and neurological deficits.
- Transcatheter aortic valve replacement (TAVR) is a relatively new, minimally invasive option that may be appropriate in patients judged to be at high-risk for traditional aortic valve surgery. It involves making a couple of tiny incisions (often just 1 to 2 inches) in blood vessels either under your left breast or in your groin; inserting long, thin tubes known as a catheters through the vessels to the aortic valve; and then—without removing the defective valve—using X-ray guidance to see inside your heart and long, thin instruments threaded through the catheters to place an artificial valve in the valvular opening. We have participated since its inception in a national clinical trial of TAVR known as the PARTNER Pivotal Trial.
In circumstances when it is appropriate, TAVR can sometimes be done with the patient under local rather than general anesthesia; in addition, it typically does not require the use of a heart-lung bypass machine. Since this approach avoids the need to open the chest at all, it usually results in much faster healing. - Composite graft surgery is an appropriate option if not only is your aortic valve damaged, but the part of your aorta closest to the heart (known as the aortic root) is affected by either an aneurysm or a dissection. This procedure involves both replacing the aortic valve with either a mechanical or a biological valve and repairing or replacing the damaged portion of the aorta itself.
What are the risks and benefits of such surgery?
It is important to keep in mind that every medical choice involves a trade-off between risks and benefits—whether it is to undergo surgery, take medication, or even just carefully monitor a condition (an option known as "watchful waiting").
In the case of a damaged or defective aortic valve, deciding whether surgery is advisable involves balancing the risks involved in any heart surgery against the risk that continuing to manage the disorder with medication and other nonsurgical treatments may result in progressive damage to your heart and circulatory system. For example, patients with a severely blocked (stenotic) aortic valve who have fainted or whose symptoms include shortness of breath or chest pain have a five-year survival rate of less than 30% without surgery.
The risks involved in surgery are far lower. A given patient's risk will vary, depending on such factors as age and overall health status, but the average mortality, or risk of death, from open surgery to repair or replace an aortic valve is from 1% to 3%. Such surgery is also associated with a 1% to 3% risk of a blood clot that causes a serious stroke. In addition, about 1% of patients may later require an artificial pacemaker. And any surgical procedure involves a very small risk of other complications, such as infection.
Patients who smoke can reduce their risk of complications if they stop smoking at least 2 to 4 weeks before their surgery (it is best not to quit immediately before having heart surgery, however, because when people stop smoking they often have short-term bronchorrhea, or excess secretions in their respiratory tract, which makes them cough a lot—and coughing a lot when you have just had heart surgery is not a good idea).
The benefits of successful surgery are considerable; repair or replacement of an aortic valve usually fixes the damaged valve and relieves all the patient's symptoms. The overwhelming majority of patients, once they recover, feel better than they did before the operation, are able to breathe far better, and are able to resume any activities they wish to engage in.
What is involved in a typical recovery?
A typical open-heart procedure takes from 4 to 6 hours, in some cases up to 8 hours; patients are then maintained under general anesthesia for an additional 4 to 6 hours. If their heart is performing well and there is no excess bleeding, they can emerge from anesthesia and have their breathing tube removed. Most patients stay in the ICU until midday of the day after their procedure; if they continue to do well, the drainage tubes in their chest can then be removed and they can be moved to a regular hospital bed later that day.
The typical hospital stay ranges from 4 to 7 days. At that point, the vast majority of patients are able to go home, with support from the visiting nurse service, though about 15% to 20% may need to spend some time in a rehab facility for more extensive rehabilitation. After discharge, patients are advised not to drive for about three weeks and not to lift anything heavier than 5 pounds for about 6 weeks. Beyond that point, they can resume whatever activities they wish to.
Patients tend to be surprised at how easy it is to control their pain. By the second day after their operation, most patients are comfortable without intravenous pain medication, taking only oral painkillers, and the overwhelming majority are discharged home on just Tylenol or Motrin.
In cases when minimally invasive surgery is appropriate, both the length of the operation and the recovery period are typically shorter (and much shorter in the case of TAVR surgery).
Page reviewed on: Jun 26, 2018
Page reviewed by: Jock McCullough, MD